Credit Balance Services
Credit balance services play a critical role in maintaining financial accuracy and compliance within healthcare organizations. When credit balances are left unresolved, they can lead to revenue leakage, patient dissatisfaction, and regulatory risk. For US healthcare providers, effective credit balance management is not just a best practice—it is a necessity.
This guide explains what credit balance services are, why they matter, and how they help healthcare organizations protect revenue and ensure compliance.
What Are Credit Balance Services?
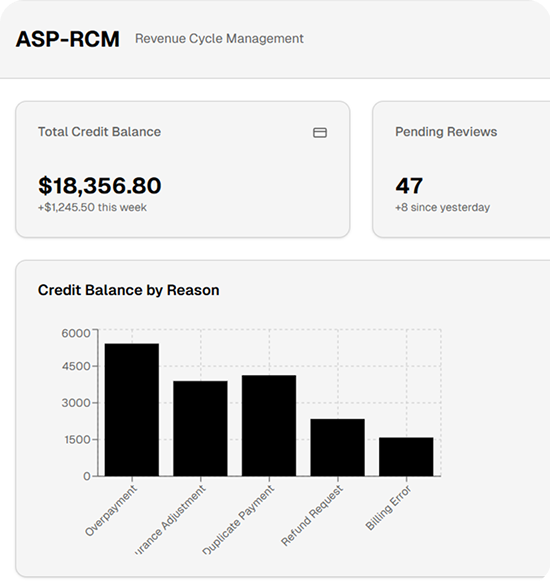
Credit balance services focus on identifying, analyzing, and resolving overpayments and negative balances in patient accounts. These balances typically occur when payments exceed charges due to insurance adjustments, duplicate payments, billing errors, or incorrect contractual allowances.
The primary goal of credit balance services is to determine whether the credit is owed to the payer or the patient and ensure timely resolution in accordance with regulatory guidelines.
Why Credit Balance Services Are Important in Healthcare
Unresolved credit balances can have serious consequences for healthcare providers. Proper credit balance management supports both financial stability and compliance.
Key Benefits of Credit Balance Services
-
Prevents revenue leakage caused by overlooked overpayments
-
Ensures compliance with CMS and payer refund regulations
-
Reduces audit risks and potential penalties
-
Improves patient trust through accurate billing practices
-
Strengthens overall revenue cycle performance
By proactively addressing credit balances, healthcare organizations can avoid costly errors and maintain clean accounts receivable.
Common Causes of Credit Balances
Understanding how credit balances occur helps providers prevent them in the future. Common causes include:
-
Duplicate insurance or patient payments
-
Incorrect charge entry or payment posting
-
Coordination of benefits errors
-
Retroactive eligibility updates
-
Over-adjustments or contractual miscalculations
Credit balance services include a thorough root-cause analysis to minimize recurring issues.
How Credit Balance Services Work
A structured credit balance review process ensures accuracy and compliance.
Step-by-Step Credit Balance Resolution Process
-
Identification – Credit balances are flagged across patient accounts
-
Validation – Payment history and payer responsibility are reviewed
-
Ownership Determination – Credit is assigned to the payer or patient
-
Refund Processing – Refunds are issued following payer and CMS rules
-
Documentation – All actions are properly recorded for audit readiness
This systematic approach helps healthcare providers maintain transparent and defensible financial records.
Credit Balance Services and Regulatory Compliance
Regulatory compliance is a major driver behind credit balance services. CMS guidelines require timely refunds for Medicare and Medicaid overpayments. Failure to comply may result in penalties, audits, or reputational damage.
Professional credit balance services ensure that healthcare providers meet federal and payer-specific regulations while maintaining proper documentation for internal and external audits.
When Should Healthcare Providers Use Credit Balance Services?
Healthcare organizations of all sizes can benefit from credit balance services, especially when:
-
Credit balances continue to age beyond 30–60 days
-
Internal teams lack time or expertise
-
Audit risk is increasing
-
Patient refund complaints rise
-
Revenue cycle inefficiencies are identified
Outsourcing or strengthening credit balance services allows internal staff to focus on core billing and collections activities.
Frequently Asked Questions (FAQs)
What is a credit balance in medical billing?
A credit balance occurs when payments exceed charges on a patient account, resulting in an overpayment that must be refunded or adjusted.
Why are credit balance services important for compliance?
They ensure timely and accurate refunds in accordance with CMS and payer regulations, reducing audit risk and penalties.
Do credit balances affect revenue?
Yes. Unresolved credit balances can distort financial reports and lead to revenue leakage if not managed correctly.
How often should credit balances be reviewed?
Most healthcare providers should conduct credit balance reviews monthly or quarterly, depending on claim volume.
Final Thoughts
Credit balance services are a vital component of effective revenue cycle management. By accurately identifying and resolving overpayments, healthcare providers can protect revenue, strengthen compliance, and enhance patient trust.
Implementing a structured and proactive credit balance strategy helps ensure financial transparency while supporting long-term operational success in today’s complex healthcare environment.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness


